Our Forgotten Organ: The Human Microbiome
by Viola Sampson
The Fulcrum, Issue 70 January 2017
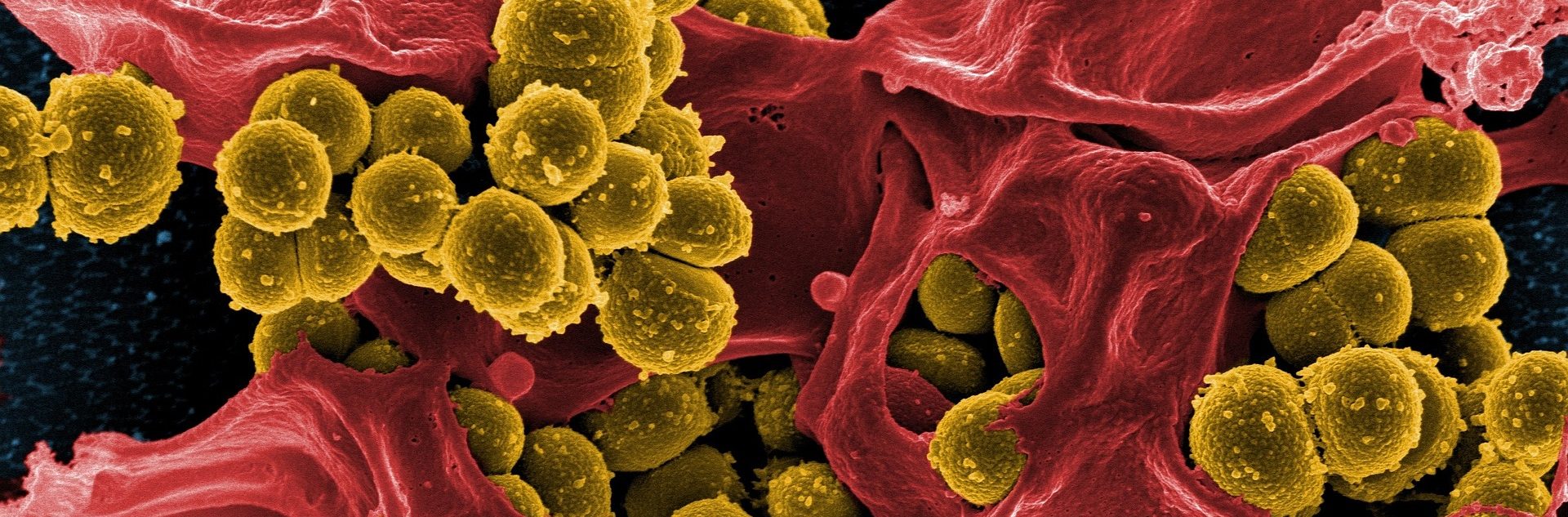
Mind-blowing new discoveries about the multitude of bacteria, viruses and fungi, living deep within and throughout the human body, are transforming the very basis of our understanding of health and disease. Disruptions in this community of microscopic life, known as the human microbiome, are now being linked to many illnesses – from asthma to obesity, from autism and IBS, to some cancers and even mental health conditions. Yet just as its huge significance is dawning on us, we are realising the microbiome is becoming dangerously degraded due to poor understanding, standard medical practices, industrialised farming, diet and lifestyle choices.
Microbes are the beginnings and the endings of the food chain: we eat them; we eat things that eat them; and they eat us when we die! They have evolved to live almost everywhere: from deep-sea volcanoes, to the stomachs of bees. Many trillions of microbes live on and in your body, and researchers are now uncovering some surprising information about them. This new knowledge has major ramifications for both complementary and conventional medical practitioners alike. The term microbe, or microorganism, simply means a life form visible only under a microscope. The term microbiome refers to the community of microbes in a particular environment, for example: the forest microbiome, or the oral microbiome. The human microbiome is made up of bacteria, archaea (that were originally thought to be bacteria, but are very different in lots of ways, and are best known for living in extreme environments), fungi (including yeasts) and single-celled amoebae, as well as viruses and bacteriophages (viruses that target bacteria). All these different microbes form diverse and interactive communities that thrive as complex ecosystems.
The human microbiome includes more than 10,000 different kinds of bacteria. Amazingly, the particular mix is unique to each individual – like a bacterial fingerprint. In your mouth, there are 700 species of bacteria – including those your dentist wants you to get rid of, but also ones that neutralise acid produced by plaque, preventing cavities. There are also amoebae hunting the bacteria between your teeth, right now, as you read this article! Researchers exploring the navel found thousands of different bacterial species live there, including 1,500 new to science, and others only previously seen in the deep ocean, in thermal vents or icebergs! On your hands, you have around 150 species of bacteria, and 30 species of fungus. Far from being dirty, it’s increasingly clear these microbes are essential to our health.
Although we have known about so-called ‘friendly bacteria’ for almost 100 years, their role in health has been a blind spot in medicine. A powerful narrative persists that healthy environments and healthy bodies are bacteria free – and this only increases with MRSA scares or E.coli outbreaks. However, understanding the microbiome may turn the current crisis of antibiotic resistance into an opportunity; revolutionising how many diseases are diagnosed and treated. Thanks to new technologies allowing scientists to identify bacteria much faster and from tiny samples, researchers are now collaborating across the globe to map the human microbiome and making some truly remarkable discoveries.
The microbiome in health and disease
We are discovering that microbes are found throughout the entire body in health, and that bacteria play major roles in a number of vital processes in the body, including manufacturing nutrients and breaking down toxins. It’s becoming clear that the microbiome influences all aspects of our physiology. About a third of metabolites in our bloodstream are now thought to be of microbial origin, influencing many organs and processes. Microbial products from the gut influence excretory processes (including bile composition), adipose tissue activity, our musculoskeletal system, endocrine system (including oestrogen levels) and circulatory system. Unexpectedly, it has emerged that bacteria and other microbes are part of our immune system – not simply in antithesis to it. For example, microbes living in our gut actually train our immune cells, while some bacteria even produce small amounts of antibiotics that kill harmful bacteria.
Changes in the microbiome are associated with an increasing number of conditions, including many we see in clinic. Research is at an early stage, and we must be careful not to attribute causality when the evidence shows only correlation, but the findings are striking nevertheless. Crohn’s Disease was one of the first conditions found to be associated with a decrease in microbial diversity in the gut. Other digestive disorders linked to changes in the microbiome, include ulcerative colitis, IBS and coeliac disease, while lung conditions include CPOD, recurrent chest infections and asthma. Because so much of our immune system is based in the gut, there’s an increasing interest in the microbiome’s role in autoimmune diseases. Studies have already found changes in the gut microbiome associated with diabetes and rheumatoid arthritis, and the absence of one particular gut bacterium has been linked with Multiple Sclerosis. Over the past year, changes in the gut microbiome have also been linked to Parkinson’s Disease. Some cancers have been linked to changes in the microbiome, including bowel cancer, and researchers are investigating the role of bacterial communities in heart disease. Premature birth now has clear association with disruptions in the microbial community of the placenta. Our gut microbiome also plays an important role in mental health, for example schizophrenia, which has been associated with the absence of a certain bacteriophage. Researchers using mice (unfortunately) have demonstrated a lack of gut microbes affects sociability, decreases memory, and increases stress responses.
The gut microbiome
Most of our microbiome is located on our skin and mucous membranes – where we meet the world – with the vast majority in the large intestine. In health, half of each stool is made up of bacteria. We have more than 1,200 species of bacteria in our gut, and there are thought to be thousands of different bacteriophages maintaining gut bacterial populations in dynamic stability. A family of archaea known as methanogens, live on waste products of the bacteria – producing the methane we release when we fart. The appendix is now thought to function as a reservoir of beneficial bacteria that repopulate the gut after an immune response, such as diarrhoea. Some of the better-studied roles of the gut microbiome include assisting nutrient absorption and producing certain hormones and vitamins (eg vitamin K, important for blood clotting). Certain gut bacteria also break down fibre in food, providing us with a tenth of our energy supply from food. Others have various immune functions: in occupying the surface of the gut, they exclude harmful bacteria; or they produce waste products and defensive products that ensure the gut suits them, not pathogenic bacteria.
The microbiome-gut-brain axis
There is now really strong evidence that our gut microbiome influences our behaviour, food cravings and mood, while our psychophysiology influences the gut and the microbiome. Researchers propose the microbiome influences the brain through several pathways, including the vagus nerve, bacterial interaction with gut endocrine cells, or through compounds produced by bacteria, such as short chain fatty acids that are directly neuroactive. Astonishingly, some bacteria have even acquired genes to produce human neurotransmitters, including GABA that affects mood. In turn, our stress hormones, including cortisol, or sympathetic neurotransmitters, influence gut motility and permeability (therefore altering the habitat of the microbiome), or some may directly influence bacterial gene expression or signalling between bacteria. Bacteria are thought to influence our behaviour and eating habits in a number of ways, including: hijacking our reward systems in our brains by producing dopamine and serotonin themselves; altering the activity of receptors in our guts and our taste buds; and releasing certain toxins in the absence of food that alter our mood.
The first thousand days of life
It’s becoming clear that how a child’s microbiome is established (seeded) has life-long consequences for health. The uterus was previously thought to be a sterile environment, however recently published research shows the placenta has a unique ecosystem of bacteria, with a surprising origin – the mother’s mouth. Researchers have also analysed meconium and the umbilical cord, showing the baby’s gut already has some bacteria before birth. However, the assumption that babies are born sterile persists even in some current medical literature.
Lactic acid-producing bacteria living on the mucous membranes of the vagina keep it acidic, preventing infection. These bacteria enter the baby’s intestines during labour and are ready to help digest lactose in breast milk. In contrast, the microbiome of caesarean babies is first colonised by the bacteria in the hospital environment and on the parents’ skin, and they also have lower bacterial diversity than vaginally-born babies. A poorly-seeded microbiome may explain the increased risk of immune system disorders, such as asthma, in people born through C-section. Recent medical trials, using vaginal swabs to seed C-section babies’ microbiomes, have had great preliminary results. Informed parents may choose to avoid prophylactic antibiotic use, ensure plenty of parental skin contact, and pack their own linen in their hospital bag.
Once born, the neonate picks up more bacteria from breast milk (ideally) and their environment, including family and pets. The microbiome continues to develop as the child grows, tries solid food and puts all manner of items in their mouth. Very recently, it was discovered that the gut microbiome undergoes a more prolonged development than previously suspected; adapting to the changing needs of the growing child. However the current consensus is that birth and the first three years of a child’s life are especially crucial. Informed parents are now questioning the trend for antimicrobial chemicals found in soaps or babies’ toys. They are thinking more carefully about chlorinated water, and about the foods they can include in their children’s diets to foster a diverse microbiome. Many promote exposure to health-promoting soil microbes, through raw, organic vegetables and outdoor play.
The role of diet: prebiotics and probiotics
There are several ways to support the health of the microbiome that lie outside the craniosacral skillset and therefore raise scope of practice issues. However, clients often talk about diet and probiotics, so it’s helpful to understand this area. A good diet includes prebiotics. These are foods that contain fibre that passes, undigested, through the upper part of the gut and stimulates the growth, activity and composition of the beneficial microbes living in the large intestine. They include onions, asparagus, pulses and Jerusalem artichokes, as well as cold potatoes and cold rice that contain resistant starches. Most of us will be familiar with a variety of probiotics – capsules, powders and liquids available from health food stores and chemists, or occasionally prescribed by progressive NHS practitioners. While poorly researched, anecdotal evidence has led to a surge in their popularity. Probiotics contain a very few microbes stable enough to survive the manufacturing process (such as Lactobacillus acidophilus and Bifidobacterium bifidum). They are almost all made up of strains of lactic acid bacteria, or just one of the many strains of beneficial yeast found in our gut (Saccharomyces boulardii). The many, many other bacteria and fungi in our microbiome just haven’t been studied enough.
Around the world, every culture has fermented foods containing bacteria, yeasts or moulds that are beneficial to us, including yoghurts, cheeses, kefir, sauerkraut, hams, olives, meads and miso. Increasingly, people are turning to these naturally probiotic foods that typically contain many more different strains of beneficial bacteria and yeasts than probiotic preparations. However, many are now pasteurised, killing the beneficial bacteria, or they are produced using commercial starter cultures that don’t have the diversity of microbes these foods once gave us. Collaborating with lactic acid bacteria naturally found in the soil and on vegetables, lacto-fermenting is the kitchen science and microbial magic in making sauerkrauts and tasty Korean pickles known as kimchi. Once part of our diets, foods like these have been disappearing ever since the invention of the fridge and tin canning. Several research papers document the health benefits of these fermented foods, while there’s much anecdotal evidence that people experience a reduction in symptoms and greater physical and emotional wellbeing once they are included in their diet.
The modern microbiome
Just as we are beginning to get to know the human microbiome, we discover we’re at a pivotal time. The human microbiome is changing rapidly, and there’s great concern that it is suffering extinctions (like other ecosystems in the wider ecological crisis). Depleted diets and excessive hygiene could be wiping out the very microbes we need for health. We also have less exposure to beneficial microbes found in soil, due to the destruction of soil fertility (which includes microbial soil life) by industrial farming methods, the increased distance from field to plate and fewer people living and working on the land. Researchers are concerned that long-term malnourishment of the microbiome, over generations, has grave consequences for the health of whole populations.
Not only food and farming practices, but also medical practices, social practices and even laws may need to change to support the human microbiome and wider microbial world.
Complementary therapists occupy an interesting place in the fertile ground of natural medicine, where we can respond to this exciting emerging field much faster than the conventional medical establishment, and help birth an even more holistic understanding of health. The microbiome should be considered in every consultation, especially in chronic and complex conditions. How might we talk with our clients about diet, lifestyle, birth and healthcare choices without contravening our code of ethics? What is our role in society more widely? What would our cranial practice look like if we recognise this fundamental aspect of our clients – and ourselves – while we work? Can we allow our perception to widen and include the microbial field? How would it be to relate to a client as a cooperative community of human cells and microbes? Understanding the microbiome locates us, and our health, as part of the wider web of life and the health of the global community of organisms. It’s time to relate to the human individual as part of a vast, invisible ecosystem – continuous with soil, sea and air.
FURTHER READING:
The Dutch microbiome museum’s beautiful website: www.micropia.nl/en/
A good, accessible introduction (although already dated): Gut: The Inside Story of Our Body’s Most Underrated Organ, by Giulia Enders, 2015, Greystone Books
A searchable, open access research journal: www.microbiomejournal.com
Find out which bacteria live in your gut and donate your microbiome sample to research! www.britishgut.org
Viola Sampson’s background is in medical research, working with bacteria in laboratory settings. Now she collaborates with bacteria in the kitchen making naturally probiotic lacto-fermented foods. She hosts an email discussion group for CAM practitioners working with the microbiome in practice (contact viola@violasampson.com), and runs lacto-fermentation workshops in London and nearby.
www.violasampson.com/wildfermentation.html
The opinions expressed in this article are those of the author and do not necessarily reflect the viewpoints of the CSTA.